We start by understanding you. We review your symptoms, medical history, lifestyle factors, and current medications. We also screen for relevant health risks (including sleep apnoea) to ensure we have the full picture.
Testosterone Replacement Therapy (TRT) & Deficiency Assessment
Doctor-led testosterone deficiency assessment and TRT management — Plymouth clinic, supporting patients across the UK (remote appointment where appropriate).
Clinically assessment by: Dr Angela Servis, Founder & Lead Practitioner (GP)
Registration: GMC reference number 6167149
Last reviewed: 18 Feb 2026
Scope: Clinical accuracy, patient safety information, and monitoring pathway.
Medical Disclaimer: This page is for general information and does not replace a medical consultation. Treatment suitability is assessed individually based on symptoms, medical history, and blood test results.
What is Testosterone Deficiency?
Testosterone deficiency (TD), also known as hypogonadism, occurs when your body produces insufficient levels of testosterone. This can impact your physical, mental, and sexual health, leading to symptoms that disrupt your daily life. Understanding and addressing these changes can significantly improve quality of life.

Common Causes
Aging
Disorders affecting the hypothalamus, pituitary glands, or testes
Chronic illnesses such as diabetes or obesity
Long-term use of medications like opiates or antipsychotics
Lifestyle factors such as poor diet, stress, or lack of physical activity
Common symptoms include:
Low mood, irritability, or reduced motivation
Reduced libido (sex drive) or erectile dysfunction
Loss of muscle mass and increased body fat
Poor concentration ("brain fog")
Why does it occur?


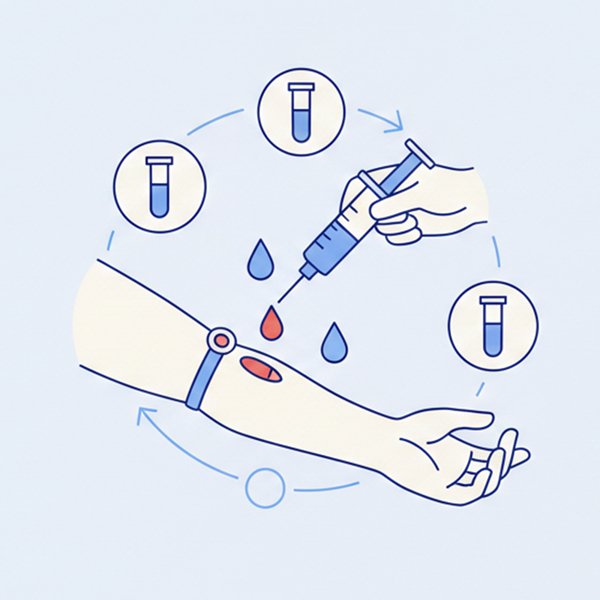
Diagnosis cannot be made on symptoms alone.
- We require venous blood samples (not finger-prick) to ensure accuracy.
- Samples should be taken between 7am – 11am (when levels are highest).
- Two separate tests are typically required to confirm a diagnosis, as testosterone levels fluctuate naturally day-to-day.
- We measure: Total & Free Testosterone, SHBG, LH, FSH, Prolactin, and general health markers (Lipids, HbA1c, PSA).

If deficient: We discuss the benefits, risks, and implications of TRT. We create a personalised plan (Gel, Injections, or HCG) that fits your lifestyle.
If not deficient: We discuss alternative causes for your symptoms and suggest other improvement strategies.
Starting treatment is just the beginning. We monitor you closely to ensure safety and effectiveness.
- Baseline: Comprehensive blood panel before starting.
- 6 Weeks: First review to check levels and adjust dose.
- 3 Months: Second review to ensure stability.
- Every 6 Months: Long-term monitoring of prostate health (PSA), blood thickness (Haematocrit), and cardiovascular health.

Treatment Options
At Eden Clinic, we offer multiple treatment options, each tailored to your lifestyle and preferences:
Our clinicians will help you decide which option best suits your needs.
Take Control of Your Hormonal Health
Understanding your testosterone levels is key to optimising your well-being. We provide simple and effective tools to help you gain insights into your hormonal health. Levels fluctuate throughout the day, so we recommend taking your blood tests between 0700-1100 in the morning to get a look at your levels when they're at their highest. It's also important to consider other factors that may have influenced your testosterone levels (recent illness, medications, significant sleep disruption).
Primary hypogonadism (PH) results from testicular dysfunction, being characterised by low testosterone and raised LH and FSH, and can be reliably diagnosed. PH isn't very common but affects 1–2% of older men. It's associated with increased risk of type 2 diabetes mellitus (T2DM) and osteoporosis.
Secondary hypogonadism (SH), sometimes called central hypogonadism, will demonstrate low testosterone with low / normal LH and FSH levels. SH is caused by dysfunction of the hypothalamo-pituitary axis. It is important to exclude haemochromatosis in these people and assess serum ferritin and pituitary hormone profile (serum prolactin, cortisol, and thyroid hormones). An MRI of the head or potentially the pituitary may be needed in some patients.
Most of the testosterone in the blood is bound to sex hormone binding globulin (SHBG), which makes it inactive. Only a small fraction exists as "free testosterone," which is biologically active and can enter cells to exert its effects around the body. Men with a body fat percentage or insulin resistance may have a very low SHBG. You can use our unit conversion tools to understand how much free testosterone you have. This can have an influence on treatment. Some blood tests don't include this separately but you can use our "free testosterone calculator' to calculate this.
Understanding the Potential Side Effects of TRT
Once starting to treat testosterone deficiency, regular monitoring is essential to manage potential side effects like acne or increased red blood cell count. It's also important to monitor your blood pressure.
Your clinician will ask you about symptoms relating to prostate health: How many times do you pass urine at night, is there any dribbling when you have finished passing water? You will also have a blood test that will monitor prostate health.
Historically there were concerns about an association with prostate cancer and men receiving TRT, however there is now good evidence that there is no association, however if you are on treatment you will be having regular blood tests.
Testosterone deficiency can negatively impact your fertility. It is worth considering this prior to starting treatment. HCG is a medication (unlicensed) that can be used to support fertility.
Injection site reactions (mild)
Male pattern baldness
Acne
Reduced fertility
Nipple tenderness or swelling (gynaecomastia)
Elevated oestrogen can cause anxiety and water retention
Prostate growth

What to Expect from TRT at Eden Clinic
Your TRT journey includes:
- Initial Consultation: A thorough assessment of your symptoms, medical history, and goals.
- Tailored Treatment Plan: Personalised recommendations based on your health profile.
- Ongoing Monitoring: Regular blood tests and follow-ups to optimise your treatment.
- Lifestyle Support: Guidance on diet, exercise, and stress management to enhance results.

Complete the ADAM Questionnaire:
Start your journey to improved health by completing our online assessment.
FAQ
Find answers to commonly asked questions about Testosterone Replacement Therapy (TRT) for men.
TRT isn’t based on symptoms alone. We assess symptoms, medical history, and blood tests to confirm whether testosterone deficiency is likely and whether TRT is appropriate.
Testing usually includes testosterone and related markers (SHBG, Albumin, LH, FSH) to interpret results in context. Additional bloods (Lipids, FBC, PSA) support safe prescribing.
Yes. Guidelines recommend at least two separate morning readings to confirm deficiency, as levels fluctuate.
There isn’t one “best” option. Gels offer steady daily levels but require daily application. Injections are less frequent but require needles. We help you choose based on your preference and response.
Yes, it can reduce sperm production. If you plan to conceive, we must discuss fertility-sparing options (like HCG) before starting.
Libido and energy often improve within weeks; body composition and mood changes may take 3-6 months of consistent treatment and lifestyle effort.
When prescribed and monitored by a doctor, it is safe. Risks (like thickened blood or prostate issues) are managed through regular blood tests.
It can. If you have undiagnosed sleep apnoea, we may recommend a sleep study or treatment alongside TRT to ensure safety.
Your natural production may take time to recover. We can guide you through a "PCT" (Post Cycle Therapy) protocol if you decide to come off treatment.
Medical References & Guidelines
We adhere to the highest standards of care, aligning with:
BSSM (British Society for Sexual Medicine): Practical Guide to Management of Testosterone Deficiency
NICE CKS: Erectile Dysfunction & Androgen Deficiency
NHS: Male Menopause Information

